Researchers Find a New Avenue to Combat Biofilm Threat
A team of researchers at The University of Texas at Austin and other institutions have unlocked a clue about how bacteria form biofilms.
U.S. Centers for Disease Control
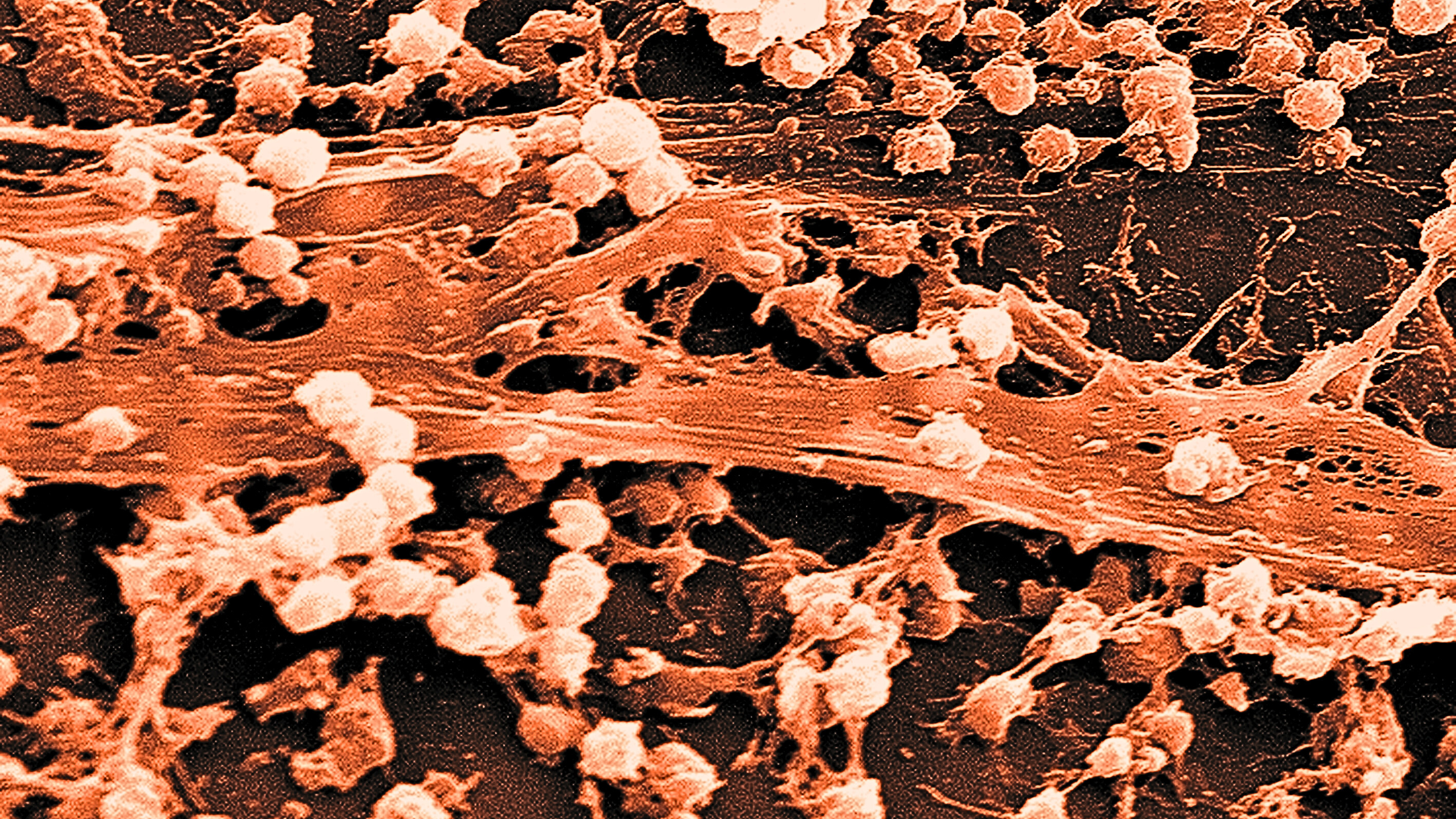
Bacterial biofilms – dense colonies of bacteria that form nearly impenetrable structures on solid surfaces – are an increasing danger. They are believed to cause millions of infections every year, leading to deaths, illness and higher health care costs, including for people with implanted medical devices.
Biofilms are particularly prevalent in medical devices inside the human body, such as knee replacements, pacemakers and catheters. Once a biofilm forms, it’s virtually impossible to get rid of. Antibiotics have no effect. Immune cells can’t combat it.
A team of researchers, led by The University of Texas at Austin’s Vernita Gordon, who also this month was named a fellow of the American Physical Society, unlocked a clue about how bacteria form biofilms. The discovery may eventually lead to new coatings on medical devices that will help put a stop to biofilm formation.
In a recent paper in npj Biofilms and Microbiomes, the team found that bacteria that land on thicker, softer gel coatings are less likely to receive the signal to start forming a biofilm when compared with bacteria on thinner, more rigid coatings.
“When bacteria encounter a solid surface, they receive signals and their gene expression changes so that they start forming biofilms,” said Gordon, an associate professor of physics at UT Austin and corresponding author of the paper. “We wanted to find out what it is about the surface that sends that signal.”
The researchers found that the bacteria experienced mechanical changes when they came into contact with certain solid surfaces. Picture the bacteria like tiny beanbags tossed on either a fluffy pillow or a cloth-covered table. Both are landing on cloth, and eventually each beanbag will squish, but the beanbag landing on the table will squish more. The more the bacteria squish, the stronger the signal that the bacteria has landed on a solid surface. That signal is what prompts the bacteria to begin to turn into a biofilm.
The team experimented with different gel coatings on rigid materials. The gels were identical on their surfaces but were different thicknesses. The researchers found that the thicker the gel, the less the bacteria experienced the mechanical changes and the less likely they were to form biofilms. The thinner films were more likely to cause the bacteria to squish and form biofilms.
“Medical devices are generally made of materials that are stiffer than the living tissues around them,” Gordon said. “There’s been a lot of discussion about coatings on devices to prevent biofilms, like antibiotics or antimicrobials. Bacteria eventually develop resistance to these, though. But what if we could prevent bacteria from ever discovering there was a solid surface there in the first place?”
That’s why Gordon and her team have focused on the physical properties of materials and how bacteria interact with them. If physical properties could be combined with antibiotics or chemical repellants, coatings on medical devices could protect against biofilms from multiple angles, making it less likely that bacteria would adapt and circumvent the preventative measures.
“We’re working to grow this research into real-world impact,” Gordon said. “The next step is to work with materials scientists and engineers to experiment with coatings on devices, and we’re looking to do that with catheters.”
Liyun Wang, Yu-Chen Wong, Joshua M. Correira, Megan Wancura, Katherine A. Brown, Berkin Dortdivanlioglu, Lauren Webb and Elizabeth Cosgriff-Hernandez of UT Austin, Chris J. Geiger, Shanice S. Webster and George A. O’Toole of Dartmouth College, Ahmed Touhami of The University of Texas Rio Grande Valley and Benjamin J. Butler and Richard M. Langford of University of Cambridge also contributed to the research. The research was funded by the Cystic Fibrosis Foundation, the National Science Foundation, the National Institutes of Health, The University of Texas Planet Texas 2050 Bridging Barriers Initiative and a UT College of Natural Sciences Spark Grant.