How a CRISPR Protein Might Yield New Tests for Many Viruses
It might enable inexpensive, highly sensitive at-home diagnostic tests for COVID-19, influenza, Ebola and more.
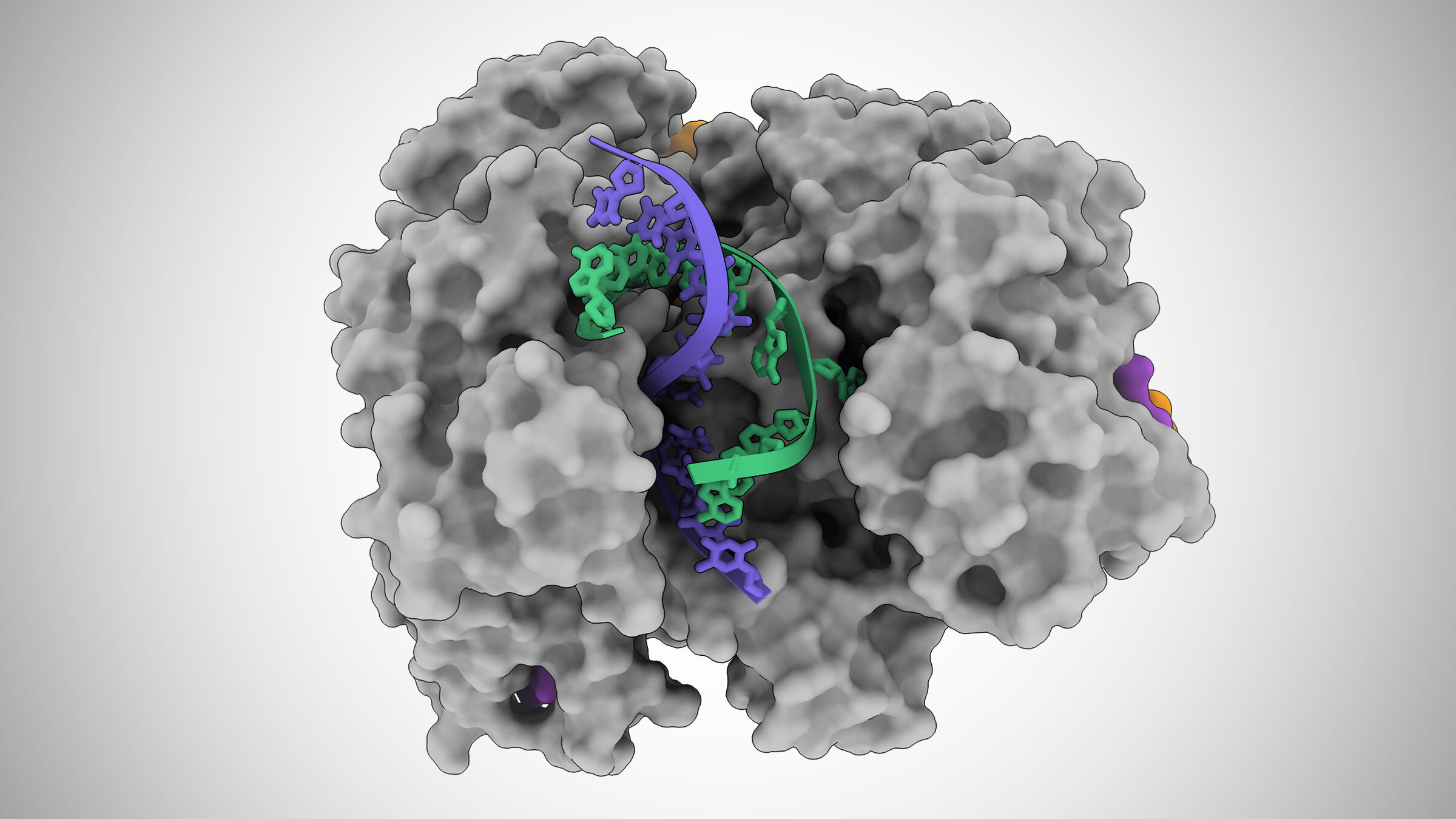
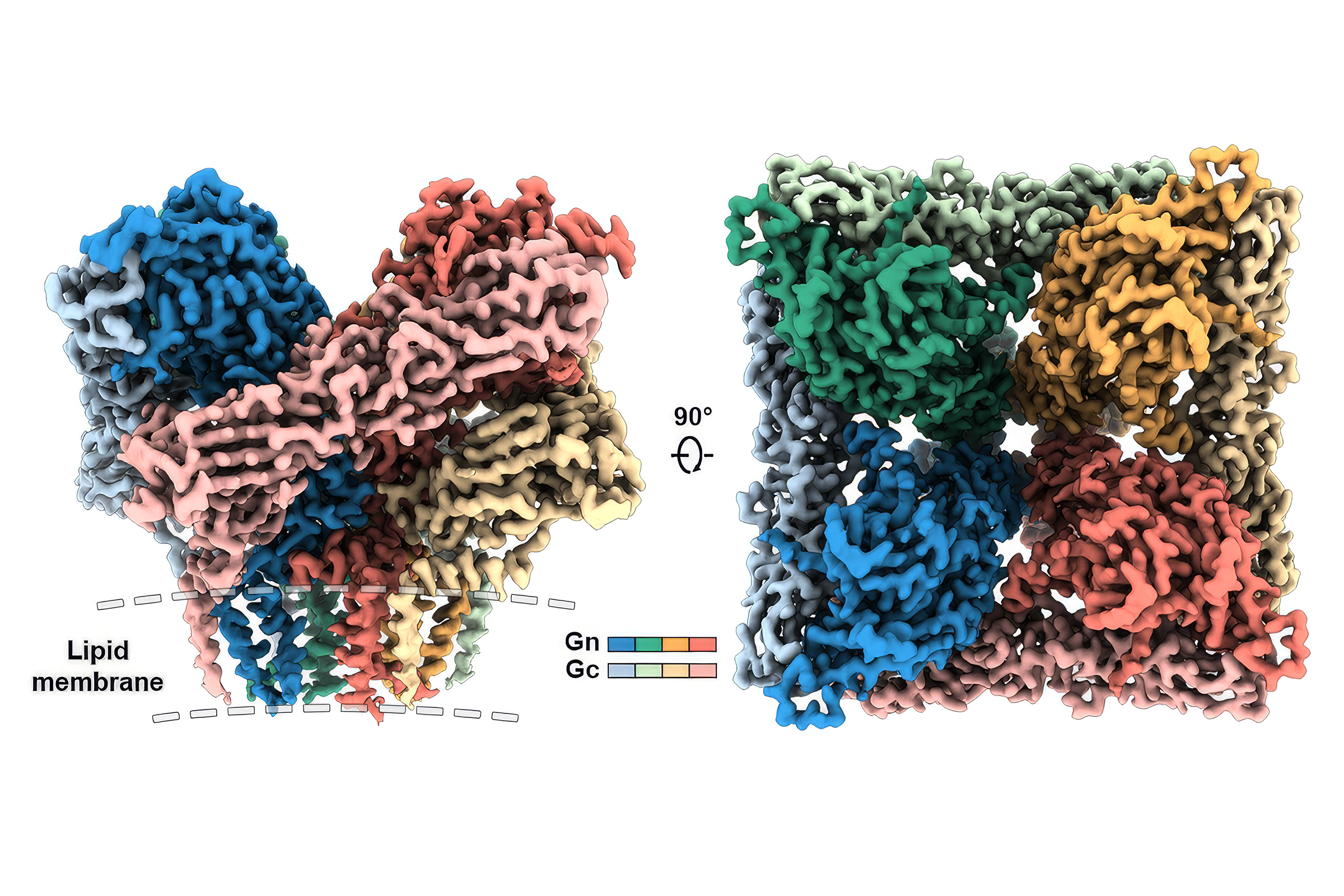
In this illustration based on cryo-electron microscope images, a Cas12a2 protein unzips a DNA double helix, allowing it to cut the single strands of DNA (blue and green). Credit: Jack Bravo/University of Texas at Austin.
In a first for the genetic toolset known as CRISPR, a recently discovered protein has been found to act as a kind of multipurpose self-destruct system for bacteria, capable of degrading single-stranded RNA, single-stranded DNA and double-stranded DNA. With its abilities to target so many types of genetic material, the discovery holds potential for the development of new inexpensive and highly sensitive at-home diagnostic tests for a wide range of infectious diseases, including COVID-19, influenza, Ebola and Zika, according to the authors of a new study in the journal Nature.
Using a high-resolution imaging technique called cryo-EM, the team discovered that when this protein, named Cas12a2, binds to a specific sequence of genetic material from a potentially dangerous virus, called a target RNA, a side portion of Cas12a2 swings out to reveal an active site, similar to a sprung-open switchblade knife. Then, the active site starts to indiscriminately cut any genetic material it comes into contact with. The researchers discovered that, with a single mutation to the Cas12a2 protein, the active site degrades only single-stranded DNA—a feature especially useful in developing new diagnostics tailored for any of a wide range of viruses.
A test based on this technology could theoretically combine the best features of PCR-based tests that detect genetic material from a virus (high sensitivity, high accuracy and the ability to detect an active infection) with the best features of rapid at-home diagnostic tests (inexpensive to produce without requiring specialized lab equipment). It also would be easily adaptable to any new RNA virus.
"If some new virus comes out tomorrow, all you have to do is figure out its genome and then change the guide RNA in your test, and you'd have a test against it," said David Taylor, an associate professor of molecular biosciences at The University of Texas at Austin and co-corresponding author of the new study.
Such a diagnostic would still require separate work and probably involve collecting saliva or a nasal sample from a patient to be mixed with the team's modified Cas12a2 protein, the piece of guide RNA that acts like a mugshot to identify a specific virus, and a fluorescent probe designed to light up when its single-stranded DNA gets cut.
CRISPR is the name for a set of tools that occur naturally in bacteria, but which scientists have adapted for use in gene editing. This is the first CRISPR protein that has been found to degrade such a wide range of genetic material.
"Cas12a2 basically grabs the two ends of the DNA double helix and bends it really tightly," said Jack Bravo, a postdoctoral fellow at UT Austin and co-first author on the paper. "And so, the helix in the middle pops open, and then this allows this active site to destroy the bits of DNA that become single-stranded. This is what makes Cas12a2 different from all the other DNA-targeting systems."
The paper's co-corresponding author is Ryan Jackson and co-first author Thomson Hallmark, both of Utah State University. The other co-authors are Bronson Naegle of Utah State and Chase Beisel of the Helmholtz Centre for Infection Research and the University of Würzburg in Germany.
Structural data were collected using the cryo-EM facilities at the Sauer Structural Biology Laboratory at The University of Texas at Austin.
Taylor, Bravo, Hallmark and Jackson are inventors on a patent application covering modifications to the Cas12a2 protein that enable it to cut only single-stranded DNA and for its use in diagnostics. Discovery to Impact, UT Austin's technology commercialization office, is managing the intellectual property and working to find industry partners that can help realize the potential of the technology.
This work was supported in part by the National Institute of General Medical Sciences of the National Institutes of Health, the German Federal Agency for Disruptive Innovation, The Welch Foundation, and the Robert J. Kleberg, Jr. and Helen C. Kleberg Foundation. David Taylor is a CPRIT scholar supported by the Cancer Prevention and Research Institute of Texas.
A companion paper in the same issue of Nature describes the biological functions of Cas12a2, while the paper described in this news release describes the mechanisms by which the protein accomplishes them.
MORE INFO
Bravo acknowledged the path to developing a diagnostic of the type Taylor described could be steep, including amid other competing diagnostics also based on CRISPR-associated proteins. Most of these have failed to make the leap from lab to the clinic, much less the home.
But these tests have challenges that the UT Austin technology would not. For example, other diagnostics, based on a CRISPR protein known as Cas13, degrade only RNA, which means that as they find target RNA, they're also destroying it, reducing the sensitivity of the tests.
"However, with our system of Cas12a2 mutants, where we can get degradation of something that is different from what we're targeting, this could lead to a really sensitive diagnostic system, because we're not depleting what we're trying to find," Bravo said.