Cancer Drug Restores Immune System’s Ability to Fight Tumors
Drug candidate developed by Everett Stone and his team is effective in mice with cancers of skin, bladder, blood and colon.
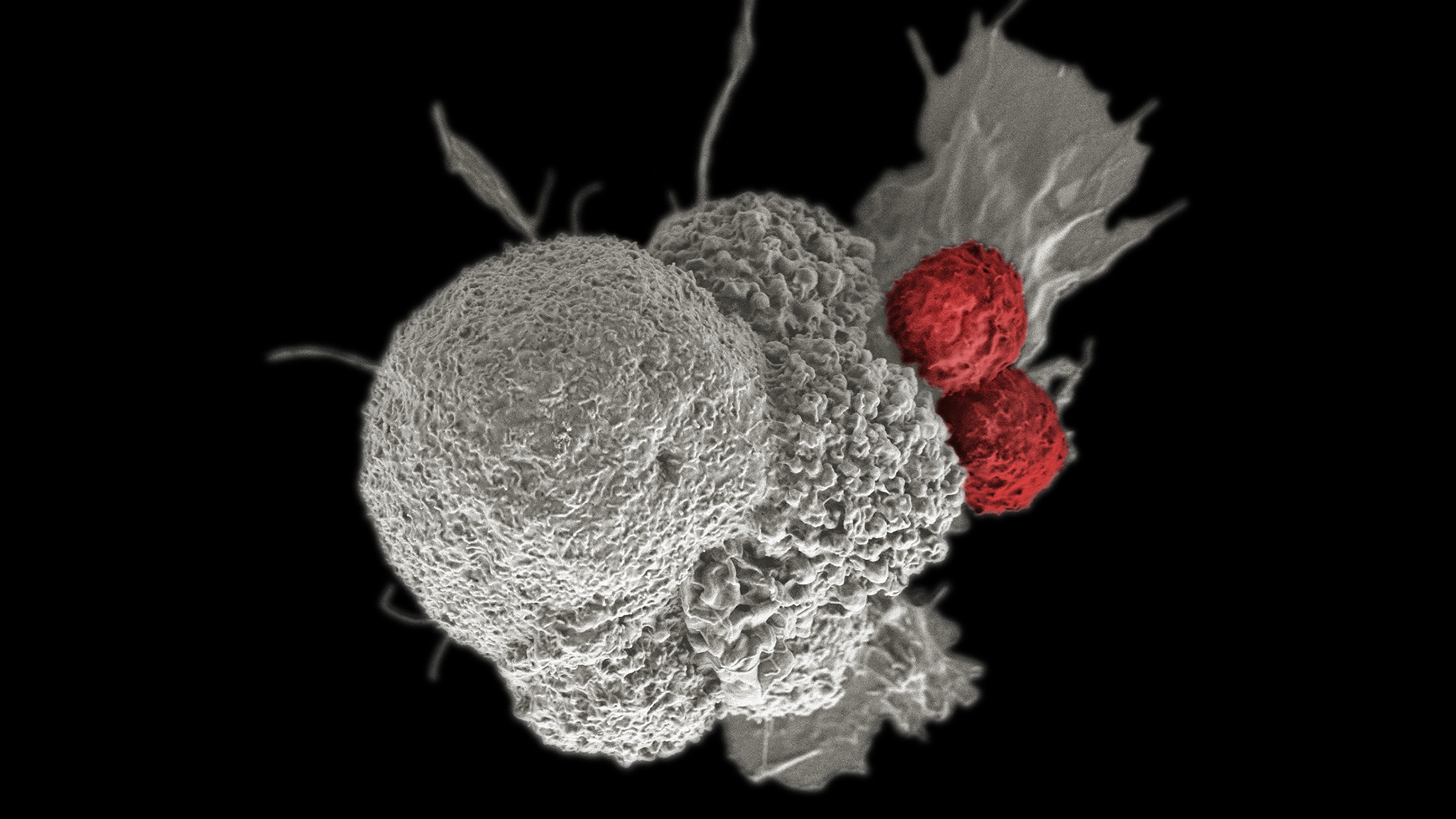
A pseudo-colored scanning electron micrograph of an oral squamous cancer cell (white) being attacked by two cytotoxic T cells (red). Credit: Rita Elena Serda, Duncan Comprehensive Cancer Center at Baylor College of Medicine, National Cancer Institute, National Institutes of Health.
A new, bio-inspired drug restores the effectiveness of immune cells in fighting cancer, a team led by researchers at The University of Texas at Austin has found. In mouse models of melanoma, bladder cancer, leukemia and colon cancer, the drug slows the growth of tumors, extends lifespan and boosts the efficacy of immunotherapy. The research is published in the journal Cancer Cell and could be a game changer for many cancer patients.
Many cancers delete a stretch of DNA called 9p21, which is the most common deletion across all cancers, occurring in 25%-50% of certain cancers such as melanoma, bladder cancer, mesothelioma and some brain cancers. Scientists have long known that cancers with the 9p21 deletion mean worse outcomes for patients and resistance to immunotherapies — the treatment strategies designed to supercharge a patient’s natural immune response to cancer.
The deletion helps cancer cells avoid getting detected and wiped out by the immune system, in part by prompting the cancer to pump out a toxic compound called MTA that impairs normal functioning of immune cells and also blocks the effectiveness of immunotherapies.
“In animal models, our drug lowers MTA back down to normal, and the immune system comes back on,” said Everett Stone, a research associate professor in the Department of Molecular Biosciences and associate professor of oncology at Dell Medical School, who led the work. “We see a lot more T cells around the tumor, and they’re in attack mode. T cells are an important immune cell type, like a SWAT team that can recognize tumor cells and pump them full of enzymes that chew up the tumor from the inside out.”
Stone envisions the drug being used in combination with immunotherapies to boost their effectiveness.
The study’s co-first authors are Donjeta Gjuka, a former UT postdoctoral researcher and currently a scientist at Takeda Oncology, and Elio Adib, formerly a postdoctoral researcher at Brigham and Women’s Hospital and the Dana-Farber Cancer Institute, and currently a resident physician at Mass General Brigham.
The 9p21 deletion leads to the loss of some key genes in cancer cells. Gone are a pair of genes that produce cell cycle regulators — proteins that keep healthy cells growing and dividing at a slow, steady rate. When those genes are lost, cells can grow unchecked. That’s what makes them cancerous. Also deleted is a housekeeping gene that produces an enzyme that breaks down the toxin MTA. It’s this loss, according to Stone, that lets cancer cells acquire a new superpower: the ability to deactivate the immune system.
“Cancer gets a two-for-one when it loses both of these genes,” Stone said. “It loses the brakes that normally keep it from growing in an uncontrolled manner. And then at the same time, it disarms the body’s police force. So, it becomes a much more aggressive and malignant kind of cancer.”
To create their drug candidate, Stone and his colleagues started with the helpful enzyme that’s naturally produced by the body to break down MTA and then added flexible polymers.
“It’s already a really good enzyme, but we needed to optimize it to last longer in the body,” Stone said. “If we injected just the natural enzyme, it would be eliminated within a few hours. In mice, our modified version stays in circulation for days; in humans it will last even longer.”
The researchers plan to do more safety tests on their drug, called PEG-MTAP, and are seeking funding to take it into human clinical trials.
The study’s other co-authors from UT are Kendra Garrison, Candice Lamb, Yuri Tanno and George Georgiou. The study’s co-corresponding authors are Stone and David Kwiatkowski, a senior physician at Brigham and Women's Hospital and a professor of medicine at Harvard Medical School.
This work was supported by funding from the National Cancer Institute, the Doris Duke Foundation, The University of Texas MD Anderson Cancer Center, the Joan and Herb Kelleher Charitable Foundation, the Kidney Cancer Association, the V Foundation and the U.S. Department of Defense.
The University of Texas at Austin is committed to transparency and disclosure of all potential conflicts of interest. University investigators involved in this research have submitted required financial disclosure forms with the University. Stone and Gjuka are inventors of two patents related to this work owned by The University of Texas at Austin.